
- During Fertility Month, IVI shares the pillars on which its success is based
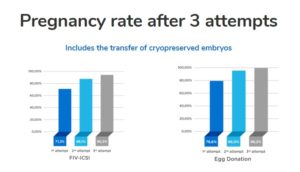
- Cumulative pregnancy rates following three IVF cycles using donated eggs are very close to 100%.
Watching over patients’ safety at every step, achieving outstanding success rates even in most challenging cases, investing in cutting-edge research and learning to control time, are four differentiating elements when offering quality assisted reproduction treatments.
Fertility Month is our month. The month when we celebrate the miracle of motherhood the most. And this year is even more special. It has been 30 years since we started making our patients’ dreams come true.
Here it is how we made it happen.
Safe assisted reproduction
We live in an age of safety, exacerbated by the most lethal pandemic of the 21st century. Resuming fertility treatments has been orchestrated by comprehensive safety measures, including over fifteen procedures that are part of the required safety protocol at all IVI clinics around the world. In addition to the basic measures (gloves, masks, protective screens, hydroalcoholic gel…), all our laboratories are equipped (and have always been equipped) with the necessary processes to work with type 2 infectious agents such as Zika or HIV and, also, SARS-CoV-2.
Likewise, given the uncertainty emerging from the COVID-19 pandemic, all our patients undergoing treatment (both women and men) are subjected to diagnostic tests at every step of the assisted reproduction process. This way, immunity is assessed and the presence of COVID-19 is ruled out. We reduce the spread of the virus while minimising the risk of patients becoming infected during their treatment.
One of the most important goals of IVI is to provide families with a healthy baby and ensure the mother-to-be stays healthy. The combination of a single embryo transfer (SET) approach and the use of preimplantation genetic testing (PGT) are two strategies that only the most specialised clinics can offer, allowing equal or greater success rates:
- A single embryo transfer policy has helped IVI to reduce twin pregnancies rates by 75% in the last ten years, which in turn reduced the maternal and foetal risks that these entail (such as prematurity, low birth weight and hypertension). At IVI, our commitment to the safety of our patients and their babies has increased our SET rates to over 98% across all treatments. We are the largest group of our kind to adopt this policy. You can see more advantages of single embryo transfer in this video:
- Similarly, using preimplantation genetic testing to rule out genetic or chromosomal abnormalities and prevent the transmission of serious genetic conditions to the offspring has increased our cumulative pregnancy rate to 73.4%.
Last but not least, the expanded carrier screening test for monogenic diseases provides life-lasting information about an individual’s reproductive risk and the chances of having a child affected by a genetic condition. In both IVF and egg donation programmes, compatibility genetic testing can be used to minimize the chance of a genetic condition being transmitted to the offspring, while giving couples the opportunity to be fully informed about their reproductive options.
Complex medical cases at IVI
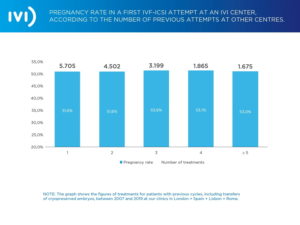
Achieving the impossible is not a pipe-dream when it comes to our pregnancy rate (see graph below). Regardless of the previous number of treatment attempts (1 to 5) a patient (or couple) have undergone before coming to IVI, the average pregnancy rate we see in complex medical cases is still over 50%.
Did you know that IVI was one of the first clinics to have its data audited by a third party? Did you know that all IVI data is validated annually, not only by a leading external auditing firm but also by the HFEA (Human Fertilisation and Embryology Authority)? This allows us to be extremely precise, and transparent, when comparing our results with those of the HFEA. These results show that IVI’s implantation rates, if you are using your own eggs, is double the national average in the UK.
Helping patients to succeed is usually not a piece of cake and we understand how long and difficult the road to motherhood can be. That’s why we try to make the experience for all of our patients as easy as possible, and give them all the support they need. We fully understand the toll that the emotional and financial burden of undergoing multiple fertility treatments can be.
Research and success rates at IVI
With more than 1,900 researchers, 28 laboratories in 9 countries and around 150 research publications per year, our only goal is to help our patients. Researching is one of the strengths and driving forces of IVI, allowing us to redefine safety standards, deliver outstanding results, and lead in the field of reproductive medicine and research. ESHRE, the highest reproductive authority in Europe, will hold its congress this year, at which IVI will be the largest group worldwide submitting over 52 scientific papers about emerging scientific reproductive topics.
Our studies and scientific research are key to achieving our success rates of 70% and 80% for IVF and egg donation, while maintaining a cumulative pregnancy rate after three attempts which is very close to 100%.
Time and age in assisted reproduction
Far from the romantic idea of holding back time, many of the advances in assisted reproduction allow us to control it. First and foremost, the AMH (anti-Müllerian hormone) test, is a blood test that assesses the ovarian reserve. For those whose biological clock is already ticking, fertility preservation or vitrification of oocytes might be the option to freeze time.
Secondly, IVI wages its own particular battle against time with several studies on ovarian rejuvenation. This technique consists of regenerating the ovarian niche by infusing platelet-rich plasma from stem-cell-rich blood. We can also activate dormant follicles by fragmenting the ovarian tissue (OFFA technique). As a result, women with very poor ovarian reserve have been able to conceive and have allowed several babies have been born. IVI London is pioneer in ovarian rejuvenation, and our results have been presented in the most important scientific meetings worldwide.
Lastly, a recent line of our research is to lengthen the telomeres (ends of the chromosomes, indicators of ageing) by applying specific medication. In other words, research is being carried out to prevent the deterioration of telomeres in patients with low ovarian reserve. This delays the ovarian ageing process and its implications for their future motherhood.
Above all, we hope that IVI’s passion for science, research, and creating life continues to allow our patients to hold their future child in their arms.




Comments are closed here.