
Sometimes, even the most advanced methods of assisted conception can benefit from an extra helping hand. Intracytoplasmic Sperm Injection (ICSI) is a procedure that is performed as part of IVF which is designed to remove barriers which can prevent a sperm cell from fertilizing an egg. For many, particularly those affected by male infertility, it can significantly improve the chances of conception.
According to the NHS, 1 in 7 couples will have difficulties when trying to conceive a child. Nearly half of these couples will find that the difficulties originate with the male partner’s sperm. This is referred to as male factor infertility. In these cases, ICSI can be performed as part of IVF treatment to increase the chances of achieving a pregnancy. It is important to remember that ICSI is not for everyone: it will not benefit all patients undergoing fertility treatment but, if male infertility is identified or there have been previous unsuccessful IVF attempts, then ICSI may be recommended to boost the chances of success.
In this article, we take a closer look at ICSI to find out:
- When is ICSI recommended, and for who?
- What should I expect if I opt for ICSI?
- Are there any risks involved with ICSI?
- What are the success rates of ICSI?
When is ICSI recommended, and for who?
As ICSI isn’t recommended for all patients, it can be added at an additional cost to your routine fertility treatment. ICSI is often recommended if:
- There is low sperm count or poor sperm mobility (poor movement);
- Sperm is abnormally shaped (poor morphology);
- Previous IVF treatments resulted in none or very few fertilized eggs;
- Surgical sperm retrieval is required (due to a medical condition, vasectomy or an extremely low sperm count);
- Embryo testing is being performed, such as Pre-Implantation Genetic Testing for Aneuploidy (PGT-A) ;
- Frozen sperm is being used that may be of low quality.
When undergoing any fertility treatment, it is normal to feel like you want to do everything you can to achieve that positive result. However, unless a male fertility issue has been identified and diagnosed, your chances of success will be the same with or without ICSI. If a fertility issue is related to poor egg quality or immature eggs failing to fertilize, then it is an issue which cannot be treated by ICSI. In these cases, you may wish to think about other options such as egg donation.
What should I expect if I opt for ICSI?
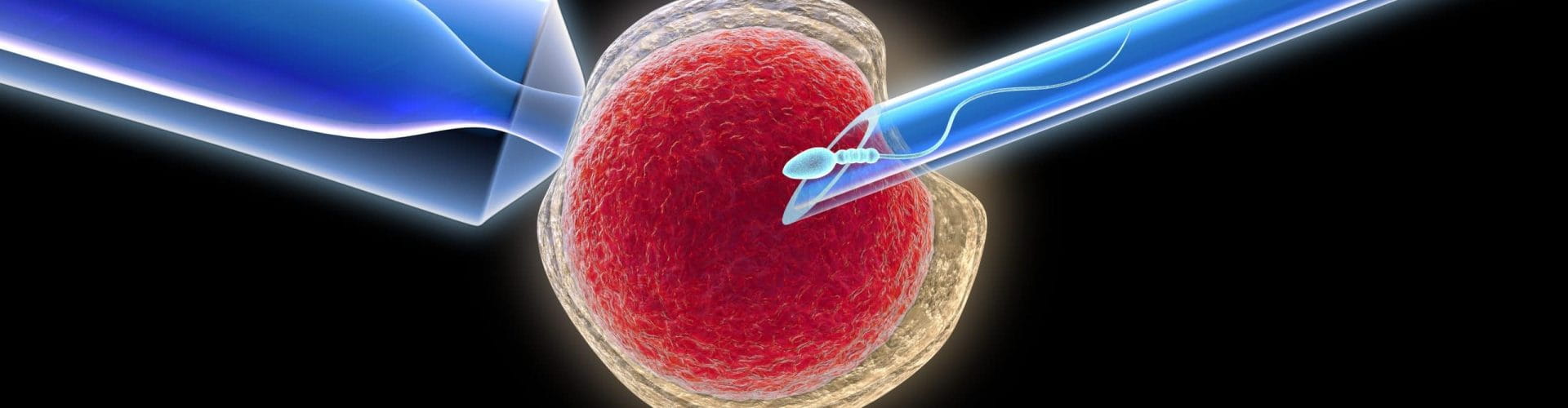
Opting for ICSI treatment will see you follow exactly the same treatment path as with conventional IVF , but a different fertilization method will be used in the laboratory. In order to fertilize an egg, the sperm must reach and attach itself to the egg and proceed to push through the harder outer layer of the egg to reach the cytoplasm. However, if the outer layer of the egg is particularly thick, or if sperm has poor mobility or abnormal morphology, this is where ICSI can increase the chances of successful fertilization.
With conventional IVF, the sperm and the egg are mixed in a petri dish and left to fertilize. With ICSI, an embryologist selects the healthiest sperm and injects the single sperm directly into the center of the egg. This helps to ensure that fertilization has the highest possible chance of occurring. It can also bypass any issues the sperm may have in reaching or penetrating the egg. Embryos are then left to develop for up to five days in a laboratory, before they are selected to be transferred to the womb with the hope of implantation.
Are there any risks involved with ICSI?
ICSI was first performed in 1987 and the technique has since advanced rapidly. As with any medical treatment, it’s not without its risks but for many people, the hope of becoming a parent outweighs the rare likelihood of these occurring. Some of the initial research into ICSI found that there is a slightly increased risk of birth defects , however this is at a level similar to conventional IVF. In both cases, the risk is just slightly higher that of a natural pregnancy in which the chances of a birth defect are between 1.5 and 3 per cent.
A 2016 study into the first offspring born as a result of ICSI found that men born using the technique had a lower quantity and quality of sperm in comparison to their naturally-conceived peers. However, this finding was not surprising to experts given that fertility issues can be hereditary. In any case, it should be noted that research is limited as the first generation of children born through ICSI only reached adulthood in 2010.
What are the success rates of ICSI?
ICSI is very effective in facilitating fertilization, but it’s important to remember that this is just one part of the IVF process. The success rate in terms of a pregnancy and live birth is still tied in with the success rate of the overall IVF treatment. The UK’s Human Fertilization & Embryology Authority (HFEA), the organization responsible for governing fertility clinics, doesn’t report separate IVF with ICSI success rates, as they are so similar to conventional IVF success rates.
While many may think that injecting the sperm directly into the egg would result in a 100 per cent success rate, this isn’t the case. While it is certainly very effective, ICSI treatment achieves successful fertilization in between 50-80 per cent of cases . The rest is down to the subsequent IVF treatment and the successful implantation of the embryo into the womb lining after being transferred.
Find Out More About ICSI Treatment
At IVI London, ISCI is just one of the fertility treatment options we offer to help our patients finally start or grow their families. Your journey with us will always start with an individual assessment so that we can recommend the fertility treatment that will be most suitable for you. If you like to learn more, why not attend one of our free online information events or speak to a member of our team to find out how we can help you.




Comments are closed here.