
ICSI vs. conventional IVF – what are the differences, what are the similarities and why choose one over the other?
If you’re interested in fertility, you’ve certainly heard of In Vitro Fertilisation (IVF) and you may have heard of the comparatively new technique of Intracytoplasmic Sperm Injection (ICSI) as a way of providing an even higher chance of fertilising an egg with sperm in the laboratory. This is true as far as it goes, but things are a little more complicated than that. It isn’t so much a matter of which is better – ICSI vs. IVF – more a matter of whether ICSI is necessary in a particular case.
In this IVI article, we unpack the difference between IVF and ICSI to help you to understand the issues that your fertility specialist will consider in deciding whether to recommend one treatment or the other, and whether it may be relevant in your circumstances.
ICSI vs conventional IVF: what are the issues?
ICSI is not a stand-alone fertility treatment in the same way as conventional IVF. It can only be used in conjunction with IVF in cases where it is necessary. In this sense, it is an add-on to IVF rather than a separate fertility treatment. Here’s what happens in both procedures:
In Vitro Fertilisation (IVF)
In conventional IVF, mature eggs are collected from the patient’s uterus following a programme of hormonal medication to stimulate the ovaries to produce multiple eggs. These are then fertilised in the laboratory, using a prepared sperm sample which is mixed together with the eggs, allowing a sperm cell, so long as it is sufficiently healthy and mobile, to penetrate the cell wall of the egg and for conception to take place. The resulting embryos are then observed as they develop for a few days in the laboratory and, when they have reached the right stage of development, the healthiest is selected for transfer to the uterus of the patient. Conventional IVF is likely to be the preferred course of treatment in certain cases of infertility:
- Couples who have tried and failed to conceive using simpler procedures such as Intrauterine Insemination (IUI)
- Women who have blocked or absent fallopian tubes
- Women who have a severe case of endometriosis
- Women of advanced maternal age, who have fewer oocytes available (low ovarian reserve)
- Couples where male factors such as poor quality sperm are the cause of infertility.
Intracytoplasmic Sperm Injection (ICSI)
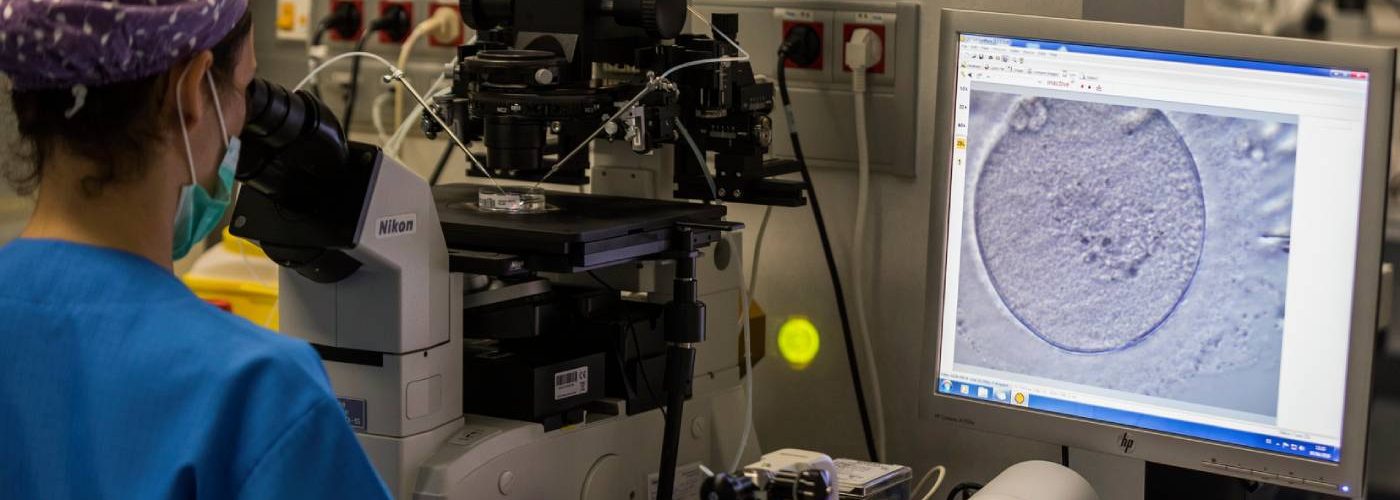
ICSI treatment follows exactly the same process as IVF up to the point where the eggs are fertilised in the laboratory. It is here that the main difference occurs. In conventional IVF, around 50,000 or more sperm are placed next to the egg in a laboratory dish. In ICSI, instead of the eggs and sperm being mixed together in a dish, embryologists select a single healthy sperm from the prepared sample. This is then micro-injected via a tiny needle called a micropipette directly through the cell wall of the egg in order for conception to take place.
This procedure is repeated for each of the available eggs. After ICSI, the pattern again reverts to the conventional IVF process and so in the same way, following ICSI, the developing embryos are observed in the laboratory and the healthiest is selected for transfer to the uterus.
When is IVF with ICSI likely to be recommended?
You can see that the ICSI process requires a lot more detailed and skilled intervention by embryologists. This means, inevitably, that it is both more time consuming and more expensive, and so we would only recommend ICSI as the preferred treatment option in certain circumstances where it significantly increases the likelihood of conception. ICSI is mostly used for couples who experience male factor fertility issues. What are these situations likely to be?
- Couples for whom conventional IVF has been previously unsuccessful
- Men with poor quality sperm due to a low sperm count, poor sperm motility or sperm morphology
- Men who have had a vasectomy. This would entail surgical retrieval of sperm from the testes, but when the quantity that can be recovered is insufficient for other procedures such as IUI or conventional IVF
- Men who have previously frozen sperm samples either before a vasectomy or before medical treatments such as radiotherapy or chemotherapy. Since the sperm available is limited, ICSI allows for its most effective use
- Women or couples where only a small number of eggs were collected following the ovarian stimulation phase
- In instances where one or both prospective parents carry a genetic disease which can be identified by pre-implantation genetic testing (PGT).
ICSI is also necessary in cases where a woman has previously frozen her eggs for the preservation of fertility, either for social reasons or medical reasons, such as having to undergo radiotherapy or chemotherapy, both of which could damage her future fertility. This is because the vitrification (freezing) process, while harmless and effective, has the effect of making the cell wall of the egg harder, so that sperm would be unable to push through into the centre of the egg (cytoplasm). Directly injecting a sperm cell into the egg using ICSI overcomes this problem.
Fertilisation success rates of ICSI
You might assume that the ICSI technique would result in 100% fertilisation rates, but this is not the case. Even when a healthy sperm is inserted directly into a healthy egg, fertilisation is not guaranteed. However, it does result in a fertilisation rate of between 50% and 80%. Once the eggs are fertilised, the success rates in terms of pregnancy are identical for both IVF and IVF with ICSI.
Learning more about IVF and ICSI
To find out more about the differences between IVF and ICSI, you are welcome to contact us to discuss your options with one of our specialists, or join a Virtual Open Evening, where you will get a chance to learn more about our treatments, and take part in a live Q&A where we can answer all of your IVF, ICSI and general fertility questions.




Comments are closed here.