
Ovarian follicles play an essential role in a woman’s fertility – both in getting pregnant and during the early stages of pregnancy. If you’re hoping to have a baby, it’s useful to have an understanding of how these follicles work.
In this article, we’ll discuss what ovarian follicles are, how they’re measured, why they’re crucial to assisted reproduction treatment, and how they factor into the chances of having a successful pregnancy.
What are ovarian follicles?
An ovarian follicle is a fluid-filled sac in which an egg grows. Once an egg reaches maturity, it is released from the follicle. This is what we know as ovulation . While most people have a good grasp of what ovulation involves, fewer may understand exactly what ovarian follicles are and their role in the process of getting pregnant.
How do ovarian follicles develop?
During each monthly menstrual cycle, women develop several follicles, measuring around 0.025 mm to begin with. Most women can expect to develop five or six follicles. Over the course of the cycle, the follicles respond to various hormones and signals that trigger their growth. In particular, the follicle stimulating hormone (FSH) , released by the pituitary gland, which causes the follicles to mature.
FSH has another important role: it also slows down the growth of the smaller follicles to allow stronger ones to thrive. As the ovarian follicles grow, they begin releasing higher amounts of estrogen . As the level of estrogenincreases, it signals to the pituitary gland to reduce FSH production. As FSH levels decline, the smaller follicles begin to stop growing as quickly (or at all), allowing the bigger, stronger follicles to carry on developing.
As the smaller follicles disintegrate, they leave behind one or two strong follicles. When fully grown, these follicles release large amounts of estrogen. This encourages the pituitary gland to start releasing luteinising hormone (LH) . This hormone is responsible for the follicle’s final development, before it bursts open to release the egg. Although it may seem like there’s a lot going on, you can trust your body knows what it’s doing! This whole process usually takes around 14 to 16 days, with the release of egg from its follicle marking ovulation .
Lifecycle of an ovarian follicle
The lifecycle of an ovarian follicle begins at birth. Women are born with a finite number of ovarian follicles, each containing a primary oocyte, or egg. Each follicle has the potential to go through its full lifecycle right through to ovulation, but only around one per cent of ovarian follicles will reach a stage to support ovulation . This means only one per cent of ovarian follicles will release an egg.
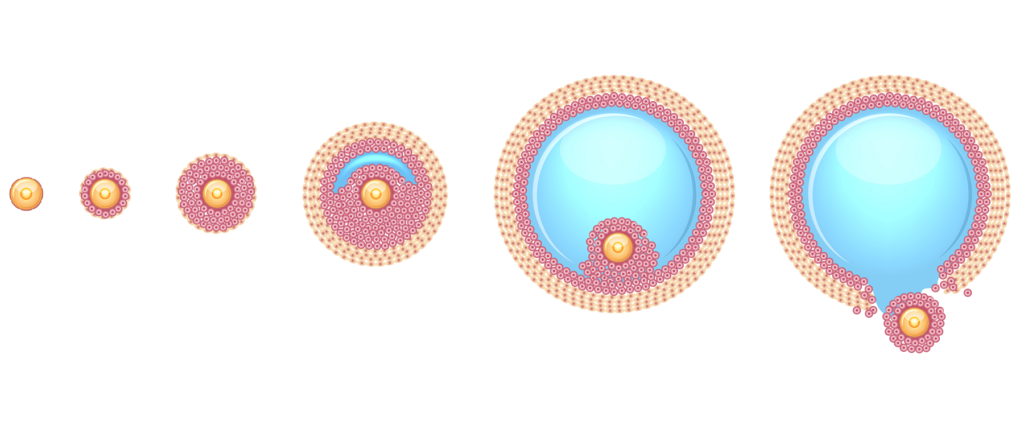
Here are the various follicular stages:
- Primordial follicle: All ovarian follicles start out here. Normally, babies are born with over a million primordial follicles, where they remain in a dormant or ‘sleeping’ state. A large number of follicles are naturally lost in this time, leaving around 300,000 upon reaching puberty.
- Primary follicle: From puberty until the menopause, the primordial follicles gradually begin to develop into primary follicles . This process takes place everyday in preparation for ovulation and can take several months. The majority do not reach maturity, after which they disintegrate and are reabsorbed into the body.
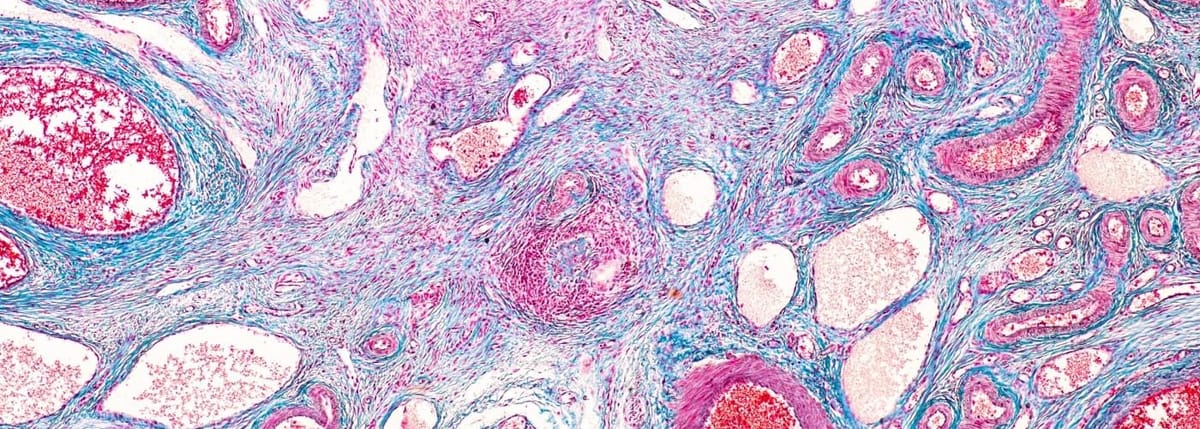
- Secondary follicle: At this stage, a layer of theca cells forms on the outside of the follicle, which contributes to the production of estrogen. Tiny pockets of nutrient-rich follicular fluid form inside the follicle, which will later form the follicle’s fluid-filled cavity (the antrum).
- Tertiary follicle : At this stage, the secondary follicle develops an antrum, forming the basic structure of a mature follicle. At this point, the follicle is at a size where it’s visible on an ultrasound scan. Follicles at the tertiary stage are also known as antral follicles .
- Graafian follicle: This is the follicular stage where the follicle is mature and ovulation is feasible. Each month, there is normally only one follicle which makes it to this stage.
- Corpus luteum: This is the last active stage of an ovarian follicle. After releasing its oocyte, post-ovulation, the corpus luteum forms from the empty follicle. The corpus luteum produces progesterone, which prompts the lining of the womb to thicken in preparation for an embryo and later, pregnancy.
While all follicles enter the primordial stage, many do not mature and only a small number will progress to the later stages.
How do ovarian follicles affect fertility?
Each ovarian follicle contains an oocyte, or an egg. The number of follicles you have is what makes up your ovarian reserve.
It is important to remember that you don’t need lots of follicles in order to have a baby. In the end, it only takes one. However, the number of follicles you have can be crucial in determining your chances of conceiving. It can also indicate whether you might need assistance in the form of a fertility treatment.
How can I find out how many follicles I have?
Unfortunately, there is no way of knowing exactly how many eggs remain in the ovary. This is because it is impossible to count the primordial follicles which contain them. Primordial follicles are microscopic: they measure only 0.025 millimetres and are too small to be seen. However, upon reaching the tertiary stage, primordial follicles grow to around 200 times their size and become visible with ultrasound technology. Unlike primordial follicles, these follicles, known as antral follicles, can be counted. An Antral Follicle Count test (AFC) is an ultrasound scan which examines each ovary and counts the number of active antral follicles that measure between 2 and 10mm. It is performed at an early stage in the menstrual cycle.
By counting the number of active antral follicles, we can calculate the ovarian reserve level. This is because the number of active antral follicles you have correlates to the number of primordial follicles that remain in the ovary.
If you have fewer antral follicles, it may mean you have a low ovarian reserve and therefore less chance of getting pregnant, naturally or with assistance. A lowered ovarian reserve is a natural part of aging. On the other hand, an unusually high number of antrum follicles could indicate an ovulation disorder such as polycystic ovarian syndrome (PCOS). So, they are a very important marker of your fertility.
Another test that can determine your egg reserve is the Anti-Müllerian Hormone (AMH) test. At the tertiary stage, antral follicles produce high levels of the anti-müllerian hormone. A simple blood test can measure this hormone to calculate your level of fertility: the more antral follicles you have, the higher the level of AMH will be circulating in your bloodstream.
Is there a fertility treatment to increase the ovarian reserve?
There is no treatment or medical intervention that can stop the natural depletion of an egg reserve, but there is hope and in this case, knowledge is power. Understanding your ovarian reserve and what it looks like gives you vital information about the steps you need to take to have a baby, when, and how.
If your ovarian reserve appears healthy and time is on your side, then we may suggest further tests to find out if there is another issue preventing you from conceiving. At this stage, it might be beneficial to consider cryopreservation of your healthy eggs through oocyte vitrification (a method of freezing eggs that maintains their quality).
If you’re considering going through In Vitro Fertilisation (IVF) treatment and have a low ovarian reserve, it is possible to encourage the ovaries to generate multiple follicles. By administering gentle hormone stimulation, we can trigger multiple follicles to mature, allowing us to retrieve a higher number of eggs. This gives you a higher likelihood of successful fertilisation in the IVF lab, resulting in more embryos available for transfer.
If you opt for Intrauterine Insemination (IUI) treatment, then one or two follicles are all that is needed. While ovarian stimulation can encourage a higher number of mature follicles to develop and increase the chances of pregnancy, you may risk complications as a result of a multiple pregnancy. Every follicle has the potential to release an egg that could then be fertilised in the womb. Once in the womb, it is impossible to control the number of eggs that get fertilised.
If you’re concerned, get in touch with our fertility specialists
At IVI, we understand the importance of an accurate diagnosis. We take an evidence-based approach to create tailor-made treatment plans, beginning with thorough diagnostic assessments for each and every patient. These tests provide crucial information that will help us build a treatment program that is highly personalized and most effective for you.
Our IVI Diagnostic Pack includes both Antral Follicle Count (AFC) and Anti-Müllerian Hormone (AMH) tests. By understanding your ovarian reserve level, it can help you plan your treatment. Contact us today and start your fertility journey.




Comments are closed here.