
Cervical cancer refers to a type of cancer that appears anywhere in the cervix – the neck of tissue that connects the vagina and uterus. Nearly all cervical cancers are caused by some type of human papillomavirus (HPV). Cervical cancers develop when cells that make up the lining of the cervix start to grow in an abnormal and uncontrolled way. A cervical screening, otherwise known as a smear or ‘pap’ test, is a common screening method to prevent cervical cancer.
A cervical screening is not designed to detect definite signs of cervical cancer or diagnose cervical cancer. A cervical screening can detect abnormal cells that show changes that could be precancerous, so they can then be removed so that they never become cancerous.
In this article, we will explain the symptoms of cervical cancer and how it is diagnosed. Around 3,200 people are diagnosed with this form of cancer in the UK each year and, as long as it is caught early, the prognosis is good.
What is HPV?
HPV is among the most common sexually-transmitted infections, with over 200 different types. Most strains are harmless and go away within one to two years. However, there are around 13 high-risk strains of HPV that, if not controlled by your immune system, can lead to cancer. Of the high-risk HPVs, HPV16 and HPV18 are responsible for the majority of cervical cancer cases. These viruses can remain in the body for many years before becoming cancerous.
The important thing to remember is that having HPV does not mean you have cancer. Indeed, HPV is so common that most sexually-active people will have come into contact with the infection at some point in their lives. However, if an HPV infection persists and worsens, you may not realise due to the absence of symptoms, which may only appear once the infection develops into cancer. That is why awareness and prevention are so important in protecting against HPV-related cancers.
How does HPV cause cervical cancer?
HPV can cause cervical cancer by triggering changes in cells in the cervix. Around 75% of cervical cancer cases develop when HPV infects the cells that line the surface of the cervix, known as squamous cells.
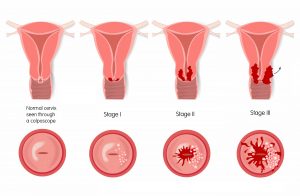
When HPV infects cervical cells, it disrupts cell DNA and changes the way cells communicate with each other, which causes them to multiply uncontrollably. As the cells multiply, they will continue to grow to form precursor lesions, called cervical intraepithelial neoplasia (CIN), which are graded based on their progression (CIN 1, 2 or 3). At this stage, it may take 10 to 30 years until the lesions become cancerous, depending on your individual risk.
Cervical cancer risk factors
You have a higher risk of developing cervical cancer if:
- You are immunocompromised: If you have a weakened immune system, your body may be less able to fight infections than someone who is not immunocompromised.
- You smoke: As Cancer Research UK warns, there is no safe level of smoking. Smoking increases your risk of lung cancer and other types of cancer, including cervical cancer.
- You became sexually active at an early age or have had multiple partners: If you have had numerous sexual partners, there is an increased risk of exposure to high-risk HPVs, like HPV16 and HPV18.
- You’ve had a baby: Women who have brought multiple pregnancies to term, or have given birth at a young age, have been shown to have an increased risk of developing cervical cancer.
- You have taken oral contraceptives: Although the connection is still unclear, studies have found an increased risk of cervical cancer in women who are using, or have used, oral contraceptives such as the pill.
- You have had chlamydia: Chlamydia bacteria helps HPV grow in the cervix, some studies have found, which may potentially increase the risk of cervical cancer.
Symptoms of cervical cancer
Cervical cancer does not always present easily identifiable symptoms, especially in the very early stages. Where no symptoms are present, you would only know if the results of your cervical screening returned as abnormal. At this stage, it can be treated easily. Where the disease does show symptoms, these may include:
- Heavier periods than usual
- Vaginal bleeding during or after sex
- Vaginal bleeding between periods
- Vaginal bleeding after menopause
Other symptoms include a vaginal discharge with an unpleasant odour, recurrent urinary tract infections (UTIs) or pain in the lower abdomen or pelvic area.
In the UK, the NHS and MacMillan Cancer Support recommend that if you experience any of these symptoms, it does not necessarily mean that you have cervical cancer. This is because these symptoms are shared with lots of other non-serious conditions. Nevertheless, you should not wait until your next cervical screening and consult your GP straight away.
How is cervical cancer diagnosed?
There is one simple diagnostic test for cervical cancer called a colposcopy. If cervical cancer cells are found, it would be followed by a series of tests. These tests will establish how far the disease has progressed. Every patient is different, and not everyone will necessarily have all the tests. However, these are some possible diagnostic steps you will need to go through.
Step-by-step cervical cancer diagnosis
- Your GP: As always, your GP is your first port of call. Your GP will likely refer you to a specialist clinic for a colposcopy. This is also the case if your cervical screening results return as abnormal.
- Colposcopy: During this procedure, a speculum is inserted into your vagina, using lubricant to avoid discomfort. The speculum expands the vagina so that the examining nurse or doctor can see your cervix. An external microscope with a light attached is used to examine the cervix. A liquid solution is applied to your cervix to help identify abnormal cells. This is safe and normally painless, but you may experience a tingling sensation. A small sample of cells may be taken for subsequent analysis in a laboratory. This is called a biopsy. A colposcopy takes between 15 and 30 minutes, and although it may be uncomfortable, it shouldn’t be painful.
- Blood tests: The colposcopy will be able to identify whether you have cervical cancer, but it will not be able to detect which stage it has reached. For this, further tests are necessary. A blood test can help in the diagnosis process through laboratory testing. The blood sample could show actual cancer cells or special proteins produced by cancer cells. It can also give your doctor an indication of how well your organs are functioning.
- Computerised tomography (CT) scan: A CT scan uses a combination of X-rays and computer modelling to provide a picture of the body’s internal structures. It can be used for diagnostic purposes alone, to determine a tumour’s exact size and location. It can also be used to enable the doctor to take a biopsy for further analysis.
- Magnetic resonance imaging (MRI) scan: An MRI scan may be performed, possibly in combination with a positron emission tomography (PET) or CT scan, or an X-ray.
- Internal examination under general anaesthetic: In some cases, an internal examination of your vagina and cervix may be required. This will be performed under general anaesthetic so you will not feel discomfort.
These tests, or combinations of tests, will establish both the exact location and size of any tumour. It will also identify the stage that the cancer has reached. The results of these diagnostic tests will provide vital information for your medical team to tailor the most effective treatment for your case.
Cancer and fertility
Unlike other cancers, cervical cancer tends to affect younger women. The majority of women diagnosed with cervical cancer are of reproductive age. Women as young as 20 can be diagnosed with cervical cancer, as well as those over the age of 60, but it is most frequently found in women between 35 and 44. This can be particularly difficult for those who have not yet started or completed their families. Depending on the severity of the cancer and your individual case, it can be possible to take steps to preserve your fertility by freezing eggs or embryos. You can read more about this in our articles about the possibilities of pregnancy after cancer and how cancer treatment affects fertility.
By preserving eggs or embryos, you can retain the possibility of using them in a future IVF treatment. If you cannot preserve fertility or in the unlikely event that your preservation treatment is not successful, then there are other ways you can build your family, such as donor egg IVF.
Getting in touch with IVI
At IVI, we are proud to lead one of the largest fertility preservation programmes for cancer patients. If you have been diagnosed with cancer, it doesn’t mean you won’t be able to have a family in the future. However, you must be informed about your fertility preservation options in the early stages of your cancer treatment. To maximise the success of your fertility preservation treatment, it must be performed before your cancer treatment begins.
Receiving news of a cancer diagnosis is a life-altering event at any age. But it is uniquely challenging for women with future plans to start a family. Although cancer treatment can affect fertility, egg or embryo freezing is a modern breakthrough allowing more and more women to preserve the possibility of becoming mothers after cancer.
If you need advice or want to discuss preserving your fertility, just get in touch with us at IVI.





Comments are closed here.