
A hysterosalpingogram, also known as uterosalpingography, is a type of specialist X-ray used to examine the shape and structure of a woman’s uterus and fallopian tubes. It is most frequently used in fertility, as it can be part of the tests done to assess couples dealing with difficulties to conceive however is not always needed if the patients are going for an IVF procedure as this treatment bypasses the tubes completely. Since its complex name, more easily abbreviated to HSG, does not give us much of an idea about what it is and how it is carried out, in this article we take a look at the details. We focus on why you may need to have this test, what the hysterosalpingogram procedure consists of and what happens afterwards. We also consider what your course of action may be if the test should confirm that you have a problem with your tubes.
There is no need to fear this fairly straightforward procedure, but it’s always good to know what to expect.
Why you may need to have a hysterosalpingogram
The NHS defines infertility as the failure to become pregnant after a year of having regular unprotected sex. It advises that this is the point when you should consult your GP about seeking help if you are under 35, or sooner if you are older.
Your GP will, of course, ask a number of questions about your health and medical history and carry out a preliminary assessment to check on possible causes of your fertility problems. At the next stage, the HSG can be one of the investigative tools needed to confirm a diagnosis. It is only one of the possible diagnostic tests; others (depending on your circumstances) could be:
- a blood test for the presence of progesterone which would confirm whether you are ovulating,
- a test for chlamydia, an STD which may have an effect on your fertility,
- an ultrasound scan to detect any endometriosis or fibroids which could be preventing conception.
What is the hysterosalpingogram procedure?
The process involves the specialist X-ray known as fluoroscopy. The uterus and fallopian tubes are filled with fluid containing a dye which can be detected by an X-ray machine, enabling the radiologist to see the inside of these organs via a TV-like monitor. From the patient point of view, the process is similar to having the annual smear test, so not exactly a bundle of fun, but reasonably tolerable. Here’s what happens.
- You lie down on a table, usually with your feet in stirrups and a speculum is inserted into your vagina, the same as for a smear test.
- An X-ray machine is lowered over your abdomen – it does not touch.
- After a swab to clean the cervix, a plastic catheter is inserted into the cervical opening; this may feel like a pap test or you may feel nothing.
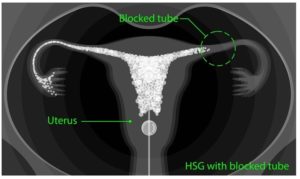
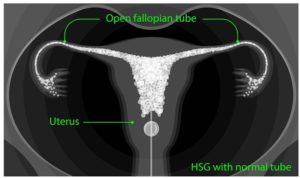
- An iodine-based dye is then injected through the catheter. This goes through the uterus, into the fallopian tubes unless they are blocked, and out into the pelvic cavity. This is what enables the radiologist to see the shape of the uterus and detect any blockages.
- X-ray pictures are taken and you may be asked to change position, perhaps on to your side. When the images are satisfactory, the machine is lifted, the speculum removed and that’s the end of the procedure.
Are there any dangers in having an HSG?
This is generally a very safe procedure but there are rare risks. There is a possibility of infection in only one per cent of cases, or a very rare allergic reaction to the iodine used. If you have fever or increasing pain following the test, or any itching or swelling, contact your doctor. The radiation used in the X-ray is of a very low dose and does not pose any threats, but it is crucial that there is no possibility of you being pregnant when the test is carried out as it could harm an unborn baby. This is why it is normally undertaken after a period and before ovulation.
Is a hysterosalpingogram painful?
In most cases, it is generally a well-tolerated procedure. If the fallopian tubes are blocked, the pressure of the liquid can cause some pain which is only brief. The upside is that in some cases, the pressure is sufficient to unblock the tubes so that a normal pregnancy is possible afterwards. There can also be mild cramping, similar to period pains, during the test.
What happens afterwards?
This is an outpatient procedure and you are free to go home afterwards. You could have mild cramps and possibly some spotting in the following days but any cramps can be treated with over-the-counter painkillers and the spotting is nothing to worry about. You are free to resume normal activities, although some doctors may advise you to refrain from sex for a few days.
What can be done if the test confirms blocked tubes?
We have seen that the hysterosalpingogram is not the only diagnostic test available but if, having been through the various procedures, it turns out that you do have issues with your tubes, it’s not the end of the story. For most people in this situation, IVF is the likely solution as this treatment bypasses the tubes completely. The only function of the fallopian tubes is the transportation of the egg, sperm and embryo. So even in the presence of blocked tubes, pregnancy would still be possible with IVF. In this well-known process, the eggs are retrieved for fertilisation and the creation of embryos happens in the laboratory. Therefore, with IVF the fallopian tubes are irrelevant as they can be bypassed. For more information on the process, take a look at our IVI video about in vitro fertilisation.
Contacting a fertility clinic
In the UK, the Human Fertilisation & Embryology Authority has some helpful advice on choosing the right clinic for you and making sure that it meets the required standards. If you decide to contact IVI, you could use our online contact form, or come to one of our Patient Open Evenings for a tour of our flagship fertility clinic. You can familiarise yourself with who we are, what we do and how we operate. It’s always good to know what to expect!





Comments are closed here.